Salivary biomarkers in non-invasive oral cancer diagnostics: a comprehensive review
DOI:
https://doi.org/10.1590/1678-7757-2024-0151Keywords:
Oral Squamous Cell Carcinoma, Saliva, Non-invasive diagnostics, Tobacco consumers, Biomarkers, Oral CancerAbstract
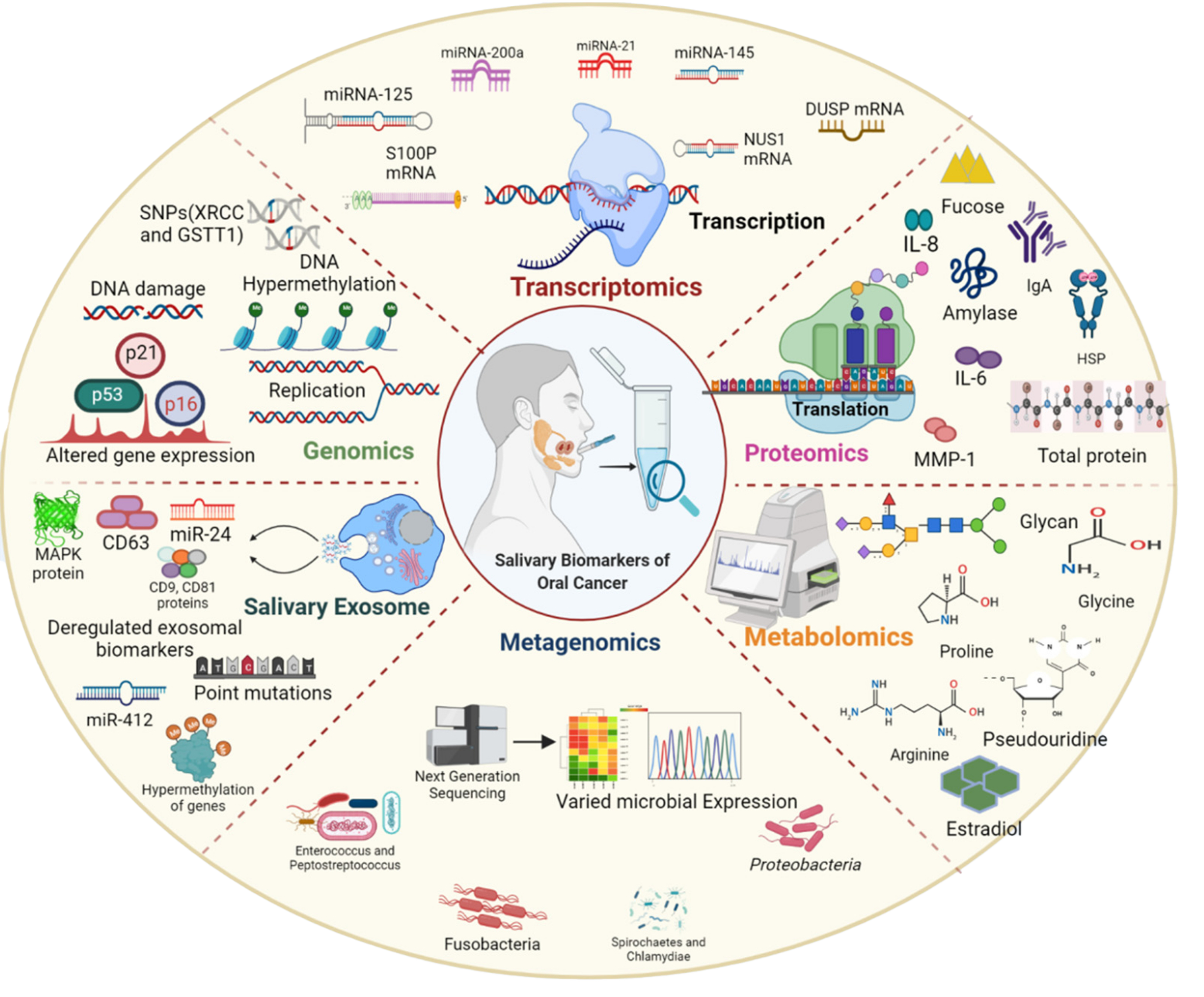
Objective: This review aims to provide a comprehensive analysis of the effectiveness of saliva as a non-invasive diagnostic marker for oral cancer. Despite progress in oral cancer diagnosis and prognosis, the 5-year survival rate remains low due to the resistance to treatment and delayed diagnosis, which can be attributed to various factors including tobacco and alcohol consumption, genetic damage, and human papillomavirus (HPV). The potential use of saliva as an easily accessible non-invasive screening and diagnostic method arises from its direct contact with the lesion site. Methodology: Data for this study were gathered via a comprehensive literature evaluation using search engines such as the PubMed, Web of Science, Google Scholar, and SciFinder. Results: Identifying salivary biomarkers shows potential to transform oral cancer diagnostics by offering a reliable alternative to the traditional invasive methods. Saliva is an abundant reservoir for both cell-bound and cell-free organic and inorganic constituents. Thus, saliva is an appropriate field for research in proteomics, genomics, metagenomics, and metabolomics. Conclusion: This review provides a comprehensive elucidation of salivary biomarkers and their function in non-invasive oral cancer diagnosis, demonstrating their potential to enhance patient outcomes and reduce the impact of this devastating disease.
Downloads
References
Yang Z, Liang X, Fu Y, Liu Y, Zheng L, Liu F, et al. Identification of AUNIP as a candidate diagnostic and prognostic biomarker for oral squamous cell carcinoma. EBioMedicine. 2019;47:44-57. doi: 10.1016/j.ebiom.2019.08.013
World Health Organization. Oral health [Internet]. Geneva: WHO; 2023 [cited 2023 Dec 29]. Available from: https://www.who.int/news-room/fact-sheets/detail/oral-health
Radhika T, Jeddy N, Nithya S, Muthumeenakshi RM. Salivary biomarkers in oral squamous cell carcinoma: an insight. J Oral Biol Craniofac Res. 2016;6(Suppl 1):S51-S54. doi: 10.1016/j.jobcr.2016.07.0034-Haghshenas MR, Moosazadeh M, Taghiloo S, Sattari S, Valadan R, Mousavi T. Association between human papillomavirus and oral cancer in iranian clinical samples: a meta-analysis review. Iran J Public Health. 2022;51(12):2688-96. doi: 10.18502/ijph.v51i12.11
Mascitti M, Orsini G, Tosco V, Monterubbianesi R, Balercia A, Putignano A, et al. An overview on current non-invasive diagnostic devices in oral oncology. Front Physiol. 2018;9:1510. doi: 10.3389/fphys.2018.01510
Khong B, Ferlito S, Quek S, Conte G, Ingrassia A, Lechien JR, et al. Past, present, and future diagnostic methods for the early noninvasive detection of oral premalignant lesions: a state of the art and systematic review. Ear Nose Throat J. 2024:1455613241245204. doi: 10.1177/01455613241245204
Bano S, David MP, Indira AP. Salivary biomarkers for oral squamous cell carcinoma: an overview. IJSS Case Rep Rev. 2015;1(8):39-45. doi: 10.17354/cr/2015/13
Majem B, Rigau M, Reventós J, Wong DT. Non-coding RNAs in saliva: emerging biomarkers for molecular diagnostics. Int J Mol Sci. 2015;16(4):8676-98. doi: 10.3390/ijms16048676
Schafer CA, Schafer JJ, Yakob M, Lima P, Camargo P, Wong DT. Saliva diagnostics: utilizing oral fluids to determine health status. Monogr Oral Sci. 2014;24:88-98. doi: 10.1159/000358791
Yoshizawa JM, Schafer CA, Schafer JJ, Farrell JJ, Paster BJ, Wong DT. Salivary biomarkers: toward future clinical and diagnostic utilities. Clin Microbiol Rev. 2013;26(4):781-91. doi: 10.1128/CMR.00021-13
Saxena S, Sankhla B, Sundaragiri KS, Bhargava A. A review of salivary biomarker: a tool for early oral cancer diagnosis. Adv Biomed Res. 2017;6:90. doi: 10.4103/2277-9175.211801
Valstar MH, Bakker BS, Steenbakkers RJ, Jong KH, Smit LA, Klein Nulent TJ, et al. The tubarial salivary glands: a potential new organ at risk for radiotherapy. Radiother Oncol. 2021;154:292-8. doi: 10.1016/j.radonc.2020.09.034
Cui Y, Yang M, Zhu J, Zhang H, Duan Z, Wang S, et al. Developments in diagnostic applications of saliva in human organ diseases. Med Nov Technol Devices. 2022;13:100115. doi: 10.1016/j.medntd.2022.100115
Carpenter GH. The secretion, components, and properties of saliva. Annu Rev Food Sci Technol. 2013;4:267-76. doi: 10.1146/annurev-food-030212-182700
Mata AD, Marques DN, Silveira JM, Marques JR, Felino ET, Guilherme NF. Effects of gustatory stimulants of salivary secretion on salivary pH and flow: a randomized controlled trial. Oral Dis. 2009;15(3):220-8. doi: 10.1111/j.1601-0825.2009.01513.x
Kaufman E, Lamster IB. The diagnostic applications of saliva: a review. Crit Rev Oral Biol Med. 2002;13(2):197-212. doi: 10.1177/154411130201300209
Kashyap B, Kullaa A. Salivary metabolites produced by oral microbes in oral diseases and oral squamous cell carcinoma: a review. Metabolites. 2024;14(5):277. doi: 10.3390/metabo14050277
Bastías D, Maturana A, Marín C, Martínez R, Niklander SE. Salivary biomarkers for oral cancer detection: an exploratory systematic review. Int J Mol Sci. 2024;25(5):2634. doi: 10.3390/ijms25052634
Halicka HD, Bedner E, Darzynkiewicz Z. Segregation of RNA and separate packaging of DNA and RNA in apoptotic bodies during apoptosis. Exp Cell Res. 2000;260(2):248-56. doi: 10.1006/excr.2000.5027
Simpson RJ, Lim JW, Moritz RL, Mathivanan S. Exosomes: proteomic insights and diagnostic potential. Expert Rev Proteomics. 2009;6(3):267-83. doi: 10.1586/epr.09.17
Sreelatha S V, Shetty S, Karnaker VK, Jacob AM, Chowdhury CR. Assaying of p53 autoantibodies in saliva for the detection of oral squamous cell carcinoma: a road not taken. Indian J Cancer [Internet]. Forthcoming 2023 [cited 2024 May 14]. Available from: https://doi.org/10.4103/ijc.ijc_870_20
Nagata S, Hamada T, Yamada N, Yokoyama S, Kitamoto S, Kanmura Y, et al. Aberrant DNA methylation of tumor-related genes in oral rinse: a noninvasive method for detection of oral squamous cell carcinoma. Cancer. 2012;118(17):4298-308. doi: 10.1002/cncr.27417
Carvalho AL, Henrique R, Jeronimo C, Nayak CS, Reddy AN, Hoque MO, et al. Detection of promoter hypermethylation in salivary rinses as a biomarker for head and neck squamous cell carcinoma surveillance. Clin Cancer Res. 2011;17(14):4782-9. doi: 10.1158/1078-0432.CCR-11-0324
Zhang X, Sjöblom T. Targeting loss of heterozygosity: a novel paradigm for cancer therapy. Pharmaceuticals (Basel). 2021;14(1):57. doi: 10.3390/ph14010057
Ambele MA, van Zyl A, Pepper MS, van Heerden MB, van Heerden WF. Amplification of 3q26.2, 5q14.3, 8q24.3, 8q22.3, and 14q32.33 are possible common genetic alterations in oral cancer patients. Front Oncol. 2020;10:683. doi: 10.3389/fonc.2020.00683
Barlebo Ahlborn L, Østrup O. Toward liquid biopsies in cancer treatment: application of circulating tumor DNA. APMIS. 2019;127(5):329-36. doi: 10.1111/apm.12912
Perdomo S, Avogbe PH, Foll M, Abedi-Ardekani B, Facciolla VL, Anantharaman D, et al. Circulating tumor DNA detection in head and neck cancer: evaluation of two different detection approaches. Oncotarget. 2017;8(42):72621-32. doi: 10.18632/oncotarget.20004
Wang Y, Springer S, Mulvey CL, Silliman N, Schaefer J, Sausen M, et al. Detection of somatic mutations and HPV in the saliva and plasma of patients with head and neck squamous cell carcinomas. Sci Transl Med. 2015;7(293):293ra104. doi: 10.1126/scitranslmed.aaa8507
Sethi S, Benninger MS, Lu M, Havard S, Worsham MJ. Noninvasive molecular detection of head and neck squamous cell carcinoma: an exploratory analysis. Diagn Mol Pathol. 2009;18(2):81-7. doi: 10.1097/PDM.0b013e3181804b82
Shah FD, Begum R, Vajaria BN, Patel KR, Patel JB, Shukla SN, et al. A review on salivary genomics and proteomics biomarkers in oral cancer. Indian J Clin Biochem. 2011;26(4):326-34. doi: 10.1007/s12291-011-0149-8
Yen CY, Liu SY, Chen CH, Tseng HF, Chuang LY, Yang CH, et al. Combinational polymorphisms of four DNA repair genes XRCC1, XRCC2, XRCC3, and XRCC4 and their association with oral cancer in Taiwan. J Oral Pathol Med. 2008;37(5):271-7. doi: 10.1111/j.1600-0714.2007.00608.x
Ranganathan K, Sivasankar V. MicroRNAs: biology and clinical applications. J Oral Maxillofac Pathol. 2014;18(2):229-34. doi: 10.4103/0973-029X.140762
Ghizoni JS, Nichele R, de Oliveira MT, Pamato S, Pereira JR. The utilization of saliva as an early diagnostic tool for oral cancer: microRNA as a biomarker. Clin Transl Oncol. 2020;22(6):804-812. doi: 10.1007/s12094-019-02210-y
Gai C, Camussi F, Broccoletti R, Gambino A, Cabras M, Molinaro L, et al. Salivary extracellular vesicle-associated miRNAs as potential biomarkers in oral squamous cell carcinoma. BMC Cancer. 2018;18(1):439. doi: 10.1186/s12885-018-4364-z
Salazar-Ruales C, Arguello JV, López-Cortés A, Cabrera-Andrade A, García-Cárdenas JM, Guevara-Ramírez P, et al. Salivary MicroRNAs for early detection of head and neck squamous cell carcinoma: a case-control study in the high altitude mestizo ecuadorian population. Biomed Res Int. 2018;2018:9792730. doi: 10.1155/2018/9792730
Yap T, Koo K, Cheng L, Vella LJ, Hill AF, Reynolds E, et al. Predicting the presence of oral squamous cell carcinoma using commonly dysregulated MicroRNA in oral swirls. Cancer Prev Res (Phila). 2018;11(8):491-502. doi: 10.1158/1940-6207.CAPR-17-0409
Al-Rawi NH, Rizvi Z, Mkadmi S, Abu Kou R, Elmabrouk N, Alrashdan MS, et al. Differential expression profile of salivary oncomirnas among smokeless tobacco users. Eur J Dent. 2023;17(4):1215-20. doi: 10.1055/s-0043-1761191
Bonne NJ, Wong DT. Salivary biomarker development using genomic, proteomic and metabolomic approaches. Genome Med. 2012;4(10):82. doi: 10.1186/gm383
Barros O, D’Agostino VG, Santos LL, Vitorino R, Ferreira R. Shaping the future of oral cancer diagnosis: advances in salivary proteomics. Expert Rev Proteomics. 2024;21(4):149-68. doi: 10.1080/14789450.2024.2343585
Riccardi G, Bellizzi MG, Fatuzzo I, Zoccali F, Cavalcanti L, Greco A, et al. Salivary biomarkers in oral squamous cell carcinoma: a proteomic overview. Proteomes. 2022;10(4):37. doi: 10.3390/proteomes10040037
Sajan T, Murthy S, Krishnankutty R, Mitra J. A rapid, early detection of oral squamous cell carcinoma: Real time PCR based detection of tetranectin. Mol Biol Res Commun. 2019;8(1):33-40. doi: 10.22099/mbrc.2019.31544.1365
Rao M, Ramesh A, Adapa S, Thomas B, Shetty J. Correlation of salivary levels of interleukin-6 and albumin with oral squamous cell carcinoma. J Health Res Rev. 2016;3(1):11-4. doi: 10.4103/2394-2010.17749
Li SX, Yang YQ, Jin LJ, Cai ZG, Sun Z. Detection of survivin, carcinoembryonic antigen and ErbB2 level in oral squamous cell carcinoma patients. Cancer Biomark. 2016;17(4):377-82. doi: 10.3233/CBM-16065144- Feng Y, Li Q, Chen J, Yi P, Xu X, Fan Y, et al. Salivary protease spectrum biomarkers of oral cancer. Int J Oral Sci. 2019;11(1):7. doi: 10.1038/s41368-018-0032-z
Ramya AS, Uppala D, Majumdar S, Surekha Ch, Deepak KG. Are salivary amylase and pH - prognostic indicators of cancers? J Oral Biol Craniofac Res. 2015;5(2):81-5. doi: 10.1016/j.jobcr.2015.04.002
Awasthi N. Role of salivary biomarkers in early detection of oral squamous cell carcinoma. Indian J Pathol Microbiol. 2017;60(4):464-8. doi: 10.4103/IJPM.IJPM_140_16
Vedam VKV, Boaz K, Natarajan S, Ganapathy S. Salivary amylase as a marker of salivary gland function in patients undergoing radiotherapy for oral cancer. J Clin Lab Anal. 2017;31(3):e22048. doi: 10.1002/jcla.2204848- Prasad G, McCullough M. Chemokines and cytokines as salivary biomarkers for the early diagnosis of oral cancer. Int J Dent. 2013;2013:813756. doi: 10.1155/2013/813756
Deepthi G, Nandan SR, Kulkarni PG. Salivary tumour necrosis factor-α as a biomarker in oral leukoplakia and oral squamous cell carcinoma. Asian Pac J Cancer Prev. 2019;20(7):2087-93. doi: 10.31557/APJCP.2019.20.7.2087
Azizi A, Dabirmoghadam P, Keykha F. Comparison of the Concentration of Salivary IL-8 in patients with oral squamous cell carcinoma and healthy subjects. J Res Dent Maxillofac Sci. 2016;1(3):28-32. doi: 10.18869/acadpub.jrdms.1.3.28
Mihara M, Shintani S, Nakahara Y, Kiyota A, Ueyama Y, Matsumura T, et al. Overexpression of CDK2 is a prognostic indicator of oral cancer progression. Jpn J Cancer Res. 2001;92(3):352-60. doi: 10.1111/j.1349-7006.2001.tb01102.x
Verma D, Garg PK, Dubey AK. Insights into the human oral microbiome. Arch Microbiol. 2018;200(4):525-40. doi: 10.1007/s00203-018-1505-3.
McLean JS. Advancements toward a systems level understanding of the human oral microbiome. Front Cell Infect Microbiol. 2014;4:98. doi: 10.3389/fcimb.2014.00098
Lee WH, Chen HM, Yang SF, Liang C, Peng CY, Lin FM, et al. Bacterial alterations in salivary microbiota and their association in oral cancer. Sci Rep. 2017;7(1):16540. doi: 10.1038/s41598-017-16418-x
Mager DL, Haffajee AD, Delvin PM, Norris CM, Posner MR, Goodson JM. The salivary microbiota as a diagnostic indicator of oral cancer: A descriptive, non-randomized study of cancer-free and oral squamous cell carcinoma subjects. J Transl Med. 2005;3:27. doi: 10.1186/1479-5876-3-27
Belibasakis GN, Senevirantne CJ, Jayasinghe RD, Vo PT, Bostanci N, Choi Y. Bacteriome and mycobiome dysbiosis in oral mucosal dysplasia and oral cancer. Periodontol 2000 [Internet]. Forthcoming 2024 [cited 2024 May 10]. Available from: https://doi.org/10.1111/prd.12558
Gopinath D, Kunnath Menon R, Chun Wie C, Banerjee M, Panda S, Mandal D, et al. Salivary bacterial shifts in oral leukoplakia resemble the dysbiotic oral cancer bacteriome. J Oral Microbiol. 2020;13(1):1857998. doi: 10.1080/20002297.2020.1857998
Yang CY, Yeh YM, Yu HY, Chin CY, Hsu CW, Liu H, et al. Oral microbiota community dynamics associated with oral squamous cell carcinoma staging. Front Microbiol. 2018;9:862. doi: 10.3389/fmicb.2018.00862
Schmidt BL, Kuczynski J, Bhattacharya A, Huey B, Corby PM, Queiroz ELS, et al. Changes in abundance of oral microbiota associated with oral cancer. PLoS One. 2014;9(6):e98741. doi: 10.1371/journal.pone.0098741
Thomas AM, Gleber-Netto FO, Fernandes GR, Amorim M, Barbosa LF, Francisco AL, et al. Alcohol and tobacco consumption affects bacterial richness in oral cavity mucosa biofilms. BMC Microbiol. 2014;14:250. doi: 10.1186/s12866-014-0250-2
Mikkonen JJ, Singh SP, Herrala M, Lappalainen R, Myllymaa S, Kullaa AM. Salivary metabolomics in the diagnosis of oral cancer and periodontal diseases. J Periodontal Res. 2016;51(4):431-7. doi: 10.1111/jre.12327
Wei J, Xie G, Zhou Z, Shi P, Qiu Y, Zheng X, et al. Salivary metabolite signatures of oral cancer and leukoplakia. Int J Cancer. 2011;129(9):2207-17. doi: 10.1002/ijc.25881
Lohavanichbutr P, Zhang Y, Wang P, Gu H, Nagana Gowda GA, Djukovic D, et al. Salivary metabolite profiling distinguishes patients with oral cavity squamous cell carcinoma from normal controls. PLoS One. 2018;13(9):e0204249. doi: 10.1371/journal.pone.0204249
Sugimoto M, Wong DT, Hirayama A, Soga T, Tomita M. Capillary electrophoresis mass spectrometry-based saliva metabolomics identified oral, breast and pancreatic cancer-specific profiles. Metabolomics. 2010;6(1):78-95. doi: 10.1007/s11306-009-0178-y
Wang Q, Gao P, Wang X, Duan Y. Investigation and identification of potential biomarkers in human saliva for the early diagnosis of oral squamous cell carcinoma. Clin Chim Acta. 2014;427:79-85. doi: 10.1016/j.cca.2013.10.00466- Wang Q, Gao P, Wang X, Duan Y. The early diagnosis and monitoring of squamous cell carcinoma via saliva metabolomics. Sci Rep. 2014;4:6802. doi: 10.1038/srep06802
Ohshima M, Sugahara K, Kasahara K, Katakura A. Metabolomic analysis of the saliva of Japanese patients with oral squamous cell carcinoma. Oncol Rep. 2017;37(5):2727-34. doi: 10.3892/or.2017.5561
Sridharan G, Ramani P, Patankar S, Vijayaraghavan R. Evaluation of salivary metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Oral Pathol Med. 2019;48(4):299-306. doi: 10.1111/jop.12835
Xiao C, Song F, Zheng YL, Lv J, Wang QF, Xu N. Exosomes in head and neck squamous cell carcinoma. Front Oncol. 2019;9:894. doi: 10.3389/fonc.2019.00894
Adeola HA, Holmes H, Temilola DO. Diagnostic potential of salivary exosomes in oral cancer. In: Sridharan G, editor. Oral cancer: current concepts and future perspectives [Internet]. London: IntechOpen; 2022 [cited 2024 July 10]. doi: 10.5772/intechopen.94192
Wang J, Jing J, Zhou C, Fan Y. Emerging roles of exosomes in oral diseases progression. Int J Oral Sci. 2024;16(1):4. doi: 10.1038/s41368-023-00274-9
Zlotogorski-Hurvitz A, Dekel BZ, Malonek D, Yahalom R, Vered M. FTIR-based spectrum of salivary exosomes coupled with computational-aided discriminating analysis in the diagnosis of oral cancer. J Cancer Res Clin Oncol. 2019;145(3):685-94. doi: 10.1007/s00432-018-02827-6
Gai C, Camussi F, Broccoletti R, Gambino A, Cabras M, Molinaro L, et al. Salivary extracellular vesicle-associated miRNAs as potential biomarkers in oral squamous cell carcinoma. BMC Cancer. 2018;18(1):439. doi: 10.1186/s12885-018-4364-z
He L, Ping F, Fan Z, Zhang C, Deng M, Cheng B, et al. Salivary exosomal miR-24-3p serves as a potential detective biomarker for oral squamous cell carcinoma screening. Biomed Pharmacother. 2020;121:109553. doi: 10.1016/j.biopha.2019.109553
Winck FV, Ribeiro AC, Domingues RR, Ling LY, Riaño-Pachón DM, Rivera C, et al. Insights into immune responses in oral cancer through proteomic analysis of saliva and salivary extracellular vesicles. Sci Rep. 2015;5:16305. doi: 10.1038/srep16305
Zlotogorski-Hurvitz A, Dayan D, Chaushu G, Salo T, Vered M. Morphological and molecular features of oral fluid-derived exosomes: oral cancer patients versus healthy individuals. J Cancer Res Clin Oncol. 2016;142(1):101-10. doi: 10.1007/s00432-015-2005-3
Arantes LM, Carvalho AC, Melendez ME, Carvalho AL. Serum, plasma and saliva biomarkers for head and neck cancer. Expert Rev Mol Diagn. 2018;18(1):85-112. doi: 10.1080/14737159.2017.1404906
Dadhich M, Prabhu V, Pai VR, D’Souza J, Harish S, Jose M. Serum and salivary sialic acid as a biomarker in oral potentially malignant disorders and oral cancer. Indian J Cancer. 2014;51(3):214-8. doi: 10.4103/0019-509X
Sartini D, Pozzi V, Renzi E, Morganti S, Rocchetti R, Rubini C, et al. Analysis of tissue and salivary nicotinamide N-methyltransferase in oral squamous cell carcinoma: basis for the development of a noninvasive diagnostic test for early-stage disease. Biol Chem. 2012;393(6):505-11. doi: 10.1515/hsz-2012-0112
Bhat S, Babu S, Bhat S, Castelino R, Rao K, Madi M. Status of serum and salivary ascorbic acid in oral potentially malignant disorders and oral cancer. Indian J Med Paediatr Oncol. 2017;38(3):306-10. doi: 10.4103/ijmpo.ijmpo_67_16
Gholizadeh N, Alipanahi Ramandi M, Motiee-Langroudi M, Jafari M, Sharouny H, Sheykhbahaei N. Serum and salivary levels of lactate dehydrogenase in oral squamous cell carcinoma, oral lichen planus and oral lichenoid reaction. BMC Oral Health. 2020;20(1):314. doi: 10.1186/s12903-020-01306-0
Dineshkumar T, Ashwini BK, Rameshkumar A, Rajashree P, Ramya R, Rajkumar K. Salivary and serum Interleukin-6 levels in Oral premalignant disorders and squamous cell carcinoma: diagnostic value and clinicopathologic correlations. Asian Pac J Cancer Prev. 2016;17(11):4899-906. doi: 10.22034/APJCP.2016.17.11.4899
Polz-Dacewicz M, Strycharz-Dudziak M, Dworzański J, Stec A, Kocot J. Salivary and serum IL-10, TNF-α, TGF-β, VEGF levels in oropharyngeal squamous cell carcinoma and correlation with HPV and EBV infections. Infect Agent Cancer. 2016;11:45. doi: 10.1186/s13027-016-0093-6
Lee LT, Wong YK, Hsiao HY, Wang YW, Chan MY, Chang KW. Evaluation of saliva and plasma cytokine biomarkers in patients with oral squamous cell carcinoma. Int J Oral Maxillofac Surg. 2018;47(6):699-707. doi: 10.1016/j.ijom.2017.09.016.
Ghanbarnia T, Seyedmajidi M, Mehryari M, Bijani A, Pooramir M, Foroughi R. Diagnostic value of serum and saliva matrix metalloproteinase13 (MMP13) in oral squamous cell carcinoma. J Babol Univ Med Sci. 2020;22:39-44.
Cao Y, Green K, Quattlebaum S, Milam B, Lu L, Gao D, et al. Methylated genomic loci encoding microRNA as a biomarker panel in tissue and saliva for head and neck squamous cell carcinoma. Clin Epigenetics. 2018;10:43. doi: 10.1186/s13148-018-0470-7
Pathiyil V, Udayasankar R. Salivary diagnostics. In: Gokul S, editor. Saliva and salivary diagnostics [Internet]. London: IntechOpen; 2019 [cited 2024 July 10]. Available from: https://dx.doi.org/10.5772/intechopen.84722
Borse V, Konwar AN, Buragohain P. Oral cancer diagnosis and perspectives in India. Sens Int. 2020;1:100046. doi: 10.1016/j.sintl.2020.10004
Kumar S, Panwar S, Kumar S, Augustine S, Malhotra BD. Biofunctionalized nanostructured yttria modified non-invasive impedometric biosensor for efficient detection of oral cancer. Nanomaterials (Basel). 2019;9(9):1190. doi: 10.3390/nano9091190
Tiwari S, Gupta PK, Bagbi Y, Sarkar T, Solanki PR. L-cysteine capped lanthanum hydroxide nanostructures for non-invasive detection of oral cancer biomarker. Biosens Bioelectron. 2017;89(Pt 2):1042-52. doi: 10.1016/j.bios.2016.10.020
Nandakumar A, Nataraj P, James A, Krishnan R, Mahesh KM. Estimation of salivary 8-Hydroxydeoxyguanosine (8-OHdG) as a potential biomarker in assessing progression towards malignancy: a case-control study. Asian Pac J Cancer Prev. 2020;21(8):2325-9. doi: 10.31557/APJCP.2020.21.8.2325
González-Pérez L, Isaza-Guzmán D, Arango-Pérez E, Tobón-Arroyave S. Analysis of salivary detection of P16INK4A and RASSF1A promoter gene methylation and its association with oral squamous cell carcinoma in a Colombian population. J Clin Exp Dent. 2020;12(5):e452-60. doi: 10.4317/jced.56647
Liyanage C, Wathupola A, Muraleetharan S, Perera K, Punyadeera C, Udagama P. Promoter hypermethylation of tumor-suppressor genes p16ink4a, RASSF1A,TIMP3, and PCQAP/MED15 in salivary dna as a quadruple biomarker panel for early detection of oral and oropharyngeal cancers. Biomolecules. 2019;9(4):148. doi: 10.3390/biom9040148.
Samadi FM, Suhail S, Sonam M, Ahmad MK, Chandra S, Saleem M. Telomerase in saliva: an assistant marker for oral squamous cell carcinoma. J Oral Maxillofac Pathol. 2019;23(2):187-91. doi: 10.4103/jomfp.JOMFP_83_19
Demokan S, Chang X, Chuang A, Mydlarz WK, Kaur J, Huang P, et al. KIF1A and EDNRB are differentially methylated in primary HNSCC and salivary rinses. Int J Cancer. 2010;127(10):2351-9. doi: 10.1002/ijc.25248
Liao PH, Chang YC, Huang MF, Tai KW, Chou MY. Mutation of p53 gene codon 63 in saliva as a molecular marker for oral squamous cell carcinomas. Oral Oncol. 2000;36(3):272-6. doi: 10.1016/s1368-8375(00)00005-1
Ovchinnikov DA, Cooper MA, Pandit P, Coman WB, Cooper-White JJ, Keith P, et al. Tumor-suppressor gene promoter hypermethylation in saliva of head and neck cancer patients. Transl Oncol. 2012;5(5):321-6. doi: 10.1593/tlo.12232
Kaliyaperumal S, Sankarapandian S. Evaluation of p16 hypermethylation in oral submucous fibrosis: a quantitative and comparative analysis in buccal cells and saliva using real-time methylation-specific polymerase chain reaction. South Asian J Cancer. 2016;5(2):73-9. doi: 10.4103/2278-330X.181645
Ovchinnikov DA, Wan Y, Coman WB, Pandit P, Cooper-White JJ, Herman JG, et al. DNA methylation at the novel CpG sites in the promoter of MED15/PCQAP gene as a biomarker for head and neck cancers. Biomark Insights. 2014;9:53-60. doi: 10.4137/BMI.S16199
Shpitzer T, Hamzany Y, Bahar G, Feinmesser R, Savulescu D, Borovoi I, et al. Salivary analysis of oral cancer biomarkers. Br J Cancer. 2009;101(7):1194-8. doi: 10.1038/sj.bjc.6605290
El-Naggar AK, Mao L, Staerkel G, Coombes MM, Tucker SL, Luna MA, et al. Genetic heterogeneity in saliva from patients with oral squamous carcinomas: implications in molecular diagnosis and screening. J Mol Diagn. 2001;3(4):164-70. doi: 10.1016/S1525-1578(10)60668-X
Don KR, Ramani P, Ramshankar V, Sherlin HJ, Premkumar P, Natesan A. Promoter hypermethylation patterns of P16, DAPK and MGMT in oral squamous cell carcinoma: a systematic review and meta-analysis. Indian J Dent Res. 2014;25(6):797-805. doi: 10.4103/0970-9290.152208
Romani C, Salviato E, Paderno A, Zanotti L, Ravaggi A, Deganello A, et al. Genome-wide study of salivary miRNAs identifies miR-423-5p as promising diagnostic and prognostic biomarker in oral squamous cell carcinoma. Theranostics. 2021;11(6):2987-99. doi: 10.7150/thno.4515
J Appl Oral Sci.104- Fadhil RS, Wei MQ, Nikolarakos D, Good D, Nair RG. Salivary microRNA miR-let-7a-5p and miR-3928 could be used as potential diagnostic bio-markers for head and neck squamous cell carcinoma. PLoS One. 2020;15(3):e0221779. doi: 10.1371/journal.pone.0221779
Du J, Gao R, Wang Y, Nguyen T, Yang F, Shi Y, et al. MicroRNA-26a/b have protective roles in oral lichen planus. Cell Death Dis. 2020;11(1):15. doi: 10.1038/s41419-019-2207-8
Uma Maheswari TN, Nivedhitha MS, Ramani P. Expression profile of salivary micro RNA-21 and 31 in oral potentially malignant disorders. Braz Oral Res. 2020;34:e002. doi: 10.1590/1807-3107bor-2020.vol34.0002
Salazar-Ruales C, Arguello JV, López-Cortés A, Cabrera-Andrade A, García-Cárdenas JM, Guevara-Ramírez P, et al. Salivary MicroRNAs for early detection of head and neck squamous cell carcinoma: a case-control study in the high altitude mestizo ecuadorian population. Biomed Res Int. 2018;2018:9792730. doi: 10.1155/2018/9792730
Gissi DB, Morandi L, Gabusi A, Tarsitano A, Marchetti C, Cura F, et al. A noninvasive test for MicroRNA expression in oral squamous cell carcinoma. Int J Mol Sci. 2018;19(6):1789. doi: 10.3390/ijms19061789
Mehdipour M, Shahidi M, Manifar S, Jafari S, Mashhadi Abbas F, Barati M, et al. Diagnostic and prognostic relevance of salivary microRNA-21, -125a, -31 and -200a levels in patients with oral lichen planus: a short report. Cell Oncol (Dordr). 2018;41(3):329-34. doi: 10.1007/s13402-018-0372-x
Shahidi M, Jafari S, Barati M, Mahdipour M, Gholami MS. Predictive value of salivary microRNA-320a, vascular endothelial growth factor receptor 2, CRP and IL-6 in Oral lichen planus progression. Inflammopharmacology. 2017;25(5):577-83. doi: 10.1007/s10787-017-0352-1
Duz MB, Karatas OF, Guzel E, Turgut NF, Yilmaz M, Creighton CJ, et al. Identification of miR-139-5p as a saliva biomarker for tongue squamous cell carcinoma: a pilot study. Cell Oncol (Dordr). 2016;39(2):187-93. doi: 10.1007/s13402-015-0259-z
Zahran F, Ghalwash D, Shaker O, Al-Johani K, Scully C. Salivary microRNAs in oral cancer. Oral Dis. 2015;21(6):739-47. doi: 10.1111/odi.12340
Momen-Heravi F, Trachtenberg AJ, Kuo WP, Cheng YS. Genomewide study of salivary MicroRNAs for detection of oral cancer. J Dent Res. 2014;93(7 Suppl):86S-93S. doi: 10.1177/0022034514531018
Salazar C, Nagadia R, Pandit P, Cooper-White J, Banerjee N, Dimitrova N, et al. A novel saliva-based microRNA biomarker panel to detect head and neck cancers. Cell Oncol (Dordr). 2014;37(5):331-8. doi: 10.1007/s13402-014-0188-2
Yang Y, Li YX, Yang X, Jiang L, Zhou ZJ, Zhu YQ. Progress risk assessment of oral premalignant lesions with saliva miRNA analysis. BMC Cancer. 2013;13:129. doi: 10.1186/1471-2407-13-129
Oh SY, Kang SM, Kang SH, Lee HJ, Kwon TG, Kim JW, et al. Potential salivary mRNA biomarkers for early detection of oral cancer. J Clin Med. 2020;9(1):243. doi: 10.3390/jcm9010243
Ueda S, Hashimoto K, Miyabe S, Hasegawa S, Goto M, Shimizu D, et al. Salivary NUS1 and RCN1 levels as biomarkers for oral squamous cell carcinoma diagnosis. In Vivo. 2020;34(5):2353-61. doi: 10.21873/invivo.12048
Michailidou E, Tzimagiorgis G, Chatzopoulou F, Vahtsevanos K, Antoniadis K, Kouidou S, et al. Salivary mRNA markers having the potential to detect oral squamous cell carcinoma segregated from oral leukoplakia with dysplasia. Cancer Epidemiol. 2016;43:112-8. doi: 10.1016/j.canep.2016.04.011
Cheng YSL, Jordan L, Rees T, Chen HS, Oxford L, Brinkmann O, et al. Levels of potential oral cancer salivary mRNA biomarkers in oral cancer patients in remission and oral lichen planus patients. Clin Oral Investig. 2014;18(3):985-93. doi: 10.1007/s00784-013-1041-0
Elashoff D, Zhou H, Reiss J, Wang J, Xiao H, Henson B, et al. Prevalidation of salivary biomarkers for oral cancer detection. Cancer Epidemiol Biomarkers Prev. 2012;21(4):664-72. doi: 10.1158/1055-9965.EPI-11-10
Cheng YS, Rees T, Wright J. A review of research on salivary biomarkers for oral cancer detection. Clin Transl Med. 2014;3(1):3. doi: 10.1186/2001-1326-3-3
Li Y, St John MA, Zhou X, Kim Y, Sinha U, Jordan RC, et al. Salivary transcriptome diagnostics for oral cancer detection. Clin Cancer Res. 2004;10(24):8442-50. doi: 10.1158/1078-0432.CCR-04-1167
Pickering V, Jordan RC, Schmidt BL. Elevated salivary endothelin levels in oral cancer patients: a pilot study. Oral Oncol. 2007;43(1):37-41. doi: 10.1016/j.oraloncology.2005.12.027
Singh P, Verma JK, Singh JK. Validation of salivary markers, IL-1β, IL-8 and Lgals3bp for detection of oral squamous cell carcinoma in an Indian population. Sci Rep. 2020;10(1):7365. doi: 10.1038/s41598-020-64494-3
Radulescu R, Greabu M, Totan A, Melescanu Imre M, Miricescu D, Didilescu A, et al. Diagnostic Role of Saliva in Oral Cancers. Rev Chim. 2020;71(7):474-80. doi: 10.37358/RC.20.7.8266
Chang YT, Chu LJ, Liu YC, Chen CJ, Wu SF, Chen CH, et al. Verification of saliva matrix metalloproteinase-1 as a strong diagnostic marker of oral cavity cancer. Cancers (Basel). 2020;12(8):2273. doi: 10.3390/cancers12082273
Smriti K, Ray M, Chatterjee T, Shenoy RP, Gadicherla S, Pentapati KC, et al. Salivary MMP-9 as a biomarker for the diagnosis of oral potentially malignant disorders and oral squamous cell carcinoma. Asian Pac J Cancer Prev. 2020;21(1):233-8. doi: 10.31557/APJCP.2020.21.1.233
Zielińska K, Karczmarek-Borowska B, Kwaśniak K, Czarnik-Kwaśniak J, Ludwin A, Lewandowski B, et al. Salivary IL-17A, IL-17F, and TNF- α Are associated with disease advancement in patients with oral and oropharyngeal cancer. J Immunol Res. 2020 Aug 13;2020:3928504. doi: 10.1155/2020/3928504
Rathore A, Katyal S, Jain A, Shetty D. Biochemical analysis of cytokeratin fragment 21-1 concentration and expression of cytokeratin 19 in oral potentially malignant disorders. J Cancer Res Ther. 2020;16(3):452-7. doi: 10.4103/jcrt.JCRT_893_17
Sami SM. Evaluation of cytokine expression tumor necrosis alpha and interleukin-6 in the saliva of oral maxillofacial benign fibro-osseous tumors and health control. Ann Trop Med Public Health. 2020;23(S13A):SP231338. doi: 10.36295/ASRO.2020.231338
Sharma M, Sharma E, Prabhu V, Pai VR, D’souza JM, Harish S, et al. Salivary L-fucose as a biomarker for oral potentially malignant disorders and oral cancer. J Cancer Res Ther. 2020;16(3):546-50. doi: 10.4103/jcrt.JCRT_552_17
Gulzar RA, Ajitha P, Subbaiyan H. Comparative evaluation on the levels of salivary Mucin MUC1 in precancerous and cancerous conditions. Int J Dentistry Oral Sci. 2021;8(8):3734-7. doi: 10.19070/2377-8075-21000765
Bhavana VS, Madhura MG, Kumar BV, Suma S, Sarita Y. Detection of salivary heat shock protein 27 by enzyme-linked immunosorbent assay and its correlation with histopathology of oral leukoplakia. J Oral Maxillofac Pathol. 2018;22(3):307-13. doi: 10.4103/jomfp.JOMFP_86_18
Bhat S, Babu GS, N. SK, Madi M, Buch S, Ullal H. Analysis and comparison of salivary L-Fucose and HSP 70 in oral potentially malignant disorders and oral cancer. Indian J Public Health Res Dev. 2020;11(2):29-33. doi: 10.37506/v11/i2/2020/ijphrd/194746
Azeem MS, Yesupatham ST, Mohiyuddin SM, Sumanth V, Ravishankar S. Usefulness of salivary sialic acid as a tumor marker in tobacco chewers with oral cancer. J Cancer Res Ther. 2020;16(3):605-11. doi: 10.4103/jcrt.JCRT_337_
Downloads
Published
Versions
- 2024-10-01 (2)
- 2024-09-11 (1)
Issue
Section
License
Copyright (c) 2024 Ravina Vats, Pooja Yadav, Afsareen Bano, Sapna Wadhwa, Rashmi Bhardwaj

This work is licensed under a Creative Commons Attribution 4.0 International License.
Todo o conteúdo do periódico, exceto onde está identificado, está licenciado sob uma Licença Creative Commons do tipo atribuição CC-BY.

