Clinical and radiographic evaluation of Bio-Oss granules and Bio-Oss Collagen in the treatment of periodontal intrabony defects
a retrospective cohort study
DOI:
https://doi.org/10.1590/1678-7757-2023-0268%20%20Keywords:
Intrabony defects, Periodontal regeneration, Bio-Oss, Bio-Oss CollagenAbstract
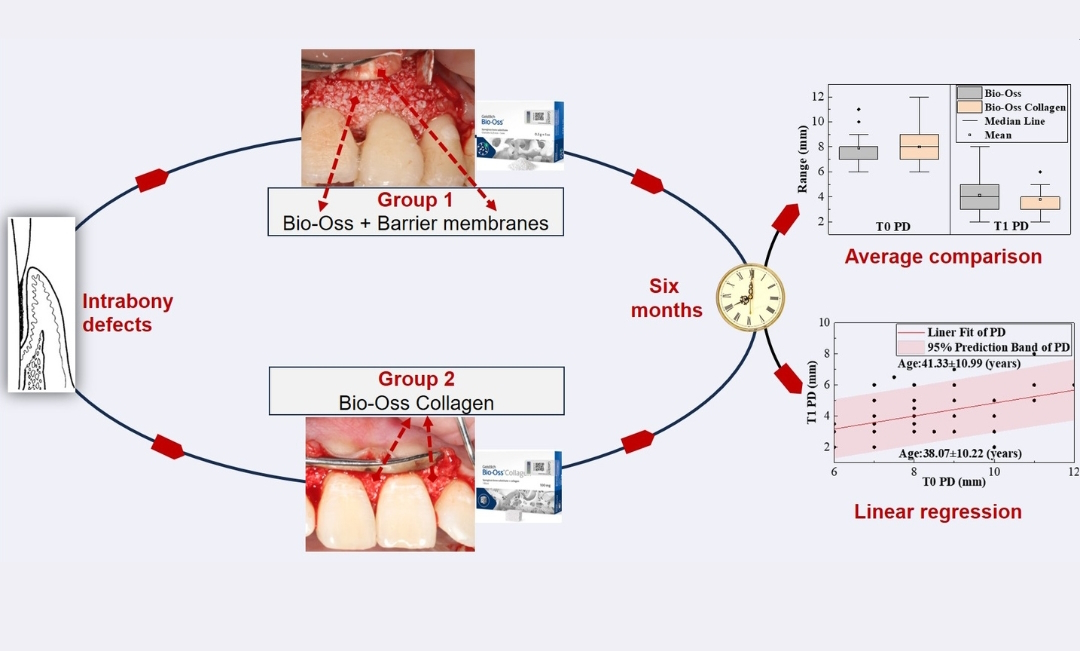
This retrospective study aimed to analyze the clinical efficacy of two regenerative surgical methods — Bio-Oss granules combined with barrier membranes and Bio-Oss Collagen alone — and to help clinicians achieve better periodontal regeneration outcomes in the specific periodontal condition. Methodology: Patients who underwent periodontal regeneration surgery from January 2018 to April 2022 were retrospectively screened, and their clinical and radiographic outcomes at 6 months postoperatively were analyzed. The probing depth (PD), clinical attachment level (CAL), bleeding on probing (BOP), gingival recession (GR), distance from the cemento-enamel junction to the bottom of the bone defect (CEJ-BD), and depth of intrabony defects (INFRA) were recorded before the operation (T0) and 6 months after it (T1), and subsequently compared. Results: In total, 143 patients were included — 77 were placed in the Bio-Oss group and 66 were placed in the Bio-Oss Collagen group. All indicators, including PD and CAL at T1, showed significant differences compared to baseline, for both groups (P<0.001). PD reduction was greater in the group receiving the Bio-Oss Collagen treatment (P=0.042). Furthermore, in cases when the baseline PD range was 7-11 mm and the age range was 35-50 years, PD reduction was more significant for patients receiving the Bio-Oss Collagen treatment (P=0.031, 0.023). A linear regression analysis indicated that postoperative PD and CAL were positively correlated with baseline values, and that the efficacy tended to decrease with increasing age. Conclusion: Both the use of Bio-Oss Collagen alone and the use of Bio-Oss granules combined with barrier membranes resulted in significant effects in the treatment of periodontal intrabony defects. The Bio-Oss Collagen treatment generated more improvements in PD than the Bio-Oss granules combined with barrier membranes, particularly within the baseline PD range of 7-11 mm and the 35-50 years age group. Additionally, age was the main factor influencing the effectiveness of regenerative surgery for intrabony defects: older individuals exhibited fewer improvements.
Downloads
References
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, et al. Periodontitis: consensus report of workgroup 2 of the 2017 World
Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol. 2018;45(Suppl 20):S162-S70. doi: 10.1111/jcpe.12946
Pilloni A, Rojas MA, Trezza C, Carere M, De Filippis A, Marsala RL, et al. Clinical effects of the adjunctive use of polynucleotide and hyaluronic acid-based gel in the subgingival re-instrumentation of residual periodontal pockets: a randomized, split-mouth clinical trial. J Periodontol. 2023;94(3):354-63. doi: 10.1002/JPER.22-0225
Matuliene G, Pjetursson BE, Salvi GE, Schmidlin K, Brägger U, Zwahlen M, et al. Influence of residual pockets on progression of periodontitis and tooth loss: results after 11 years of maintenance.J Clin Periodontol. 2008;35(8):685-95. doi: 10.1111/j.1600-051X.2008.01245.x
Castro AB, Meschi N, Temmerman A, Pinto N, Lambrechts P, Teughels W, et al. Regenerative potential of leucocyte- and platelet-rich fibrin.
Part A: intra-bony defects, furcation defects and periodontal plastic surgery. A systematic review and meta-analysis. J Clin Periodontol. 2017;44(1):67-82. doi: 10.1111/jcpe.12643
Nibali L, Koidou VP, Nieri M, Barbato L, Pagliaro U, Cairo F. Regenerative surgery versus access flap for the treatment of intra-
bony periodontal defects: a systematic review and meta-analysis. J Clin Periodontol. 2020;47(Suppl 22):320-51. doi: 10.1111/jcpe.13237
Kao RT, Nares S, Reynolds MA. Periodontal regeneration - intrabony defects: a systematic review from the AAP Regeneration
Workshop. J Periodontol. 2015;86(Suppl 2):S77-104. doi: 10.1902/jop.2015.130685
Anoixiadou S, Parashis A, Vouros I. Minimally invasive non-surgical technique in the treatment of intrabony defects-a narrative review. Dent J (Basel). 2023;11(1):25. doi: 10.3390/dj11010025
Cortellini P, Cortellini S, Bonaccini D, Tonetti MS. Modified minimally invasive surgical technique in human intrabony defects with or without regenerative materials-10-year follow-up of a randomized clinical trial: Tooth retention, periodontitis recurrence, and costs. J Clin Periodontol. 2022;49(6):528-36. doi: 10.1111/jcpe.13627
Deng Y, Liang Y, Liu X. Biomaterials for periodontal regeneration. Dent Clin North Am. 2022;66(4):659-72. doi: 10.1016/j.cden.2022.05.011
Elgali I, Omar O, Dahlin C, Thomsen P. Guided bone regeneration: materials and biological mechanisms revisited. Eur J Oral Sci.
;125(5):315-37. doi: 10.1111/eos.12364
Starch-Jensen T, Bruun NH, Spin-Neto R. Endo-sinus bone gain following osteotome-mediated sinus floor elevation with Bio-Oss Collagen compared with no grafting material: a one-year single-blind randomized controlled trial. Int J Oral Maxillofac Surg.
;52(11):1205-15. doi: 10.1016/j.ijom.2023.03.009
Pang KM, Um IW, Kim YK, Woo JM, Kim SM, Lee JH. Autogenous demineralized dentin matrix from extracted tooth for the augmentation
of alveolar bone defect: a prospective randomized clinical trial in comparison with anorganic bovine bone. Clin Oral Implants Res. 2017;28(7):809-15. doi: 10.1111/clr.12885
Kim SE, Lee E, Jang K, Shim KM, Kang SS. Evaluation of porcine hybrid bone block for bone grafting in dentistry. In Vivo. 2018;32(6):1419-26. doi: 10.21873/invivo.11394
Ying Y, Li B, Liu C, Xiong Z, Bai W, Li J, Ma P. A biodegradable gelatin-based nanostructured sponge with space maintenance to
enhance long-term osteogenesis in maxillary sinus augmentation. J Biomater Appl. 2021;35(6):681-95. doi: 10.1177/0885328220964446
Hartman GA, Arnold RM, Mills MP, Cochran DL, Mellonig JT. Clinical and histologic evaluation of anorganic bovine bone collagen with or without a collagen barrier. Int J Periodontics Restorative Dent. 2004;24(2):127-35.
Couso-Queiruga E, Weber HA, Garaicoa-Pazmino C, Barwacz C, Kalleme M, Galindo-Moreno P, et al. Influence of healing time on
the outcomes of alveolar ridge preservation using a collagenated bovine bone xenograft: a randomized clinical trial. J Clin Periodontol.
;50(2):132-46. doi:10.1111/jcpe.13744
Han HS, Lee JT, Oh S, Cho YD, Kim S. Evaluation of alveolar ridge preservation in sockets with buccal dehiscence defects using two types
of xenogeneic biomaterials: an in vivo experimental study. Clin Oral Implants Res. 2023;34(11):1289-98. doi:10.1111/clr.14169
De Bruyckere T, Eghbali A, Younes F, Cleymaet R, Jacquet W, De Bruyn H, et al. A 5-year prospective study on regenerative periodontal therapy of infrabony defects using minimally invasive surgery and a collagen-enriched bovine-derived xenograft. Clin Oral Investig.
;22(3):1235-42. doi:10.1007/s00784-017-2208-x
Nevins ML, Camelo M, Rebaudi A, Lynch SE, Nevins M. Three-dimensional micro-computed tomographic evaluation of periodontal
regeneration: a human report of intrabony defects treated with Bio-Oss collagen. Int J Periodontics Restorative Dent. 2005;25(4):365-73.
- Xu D, Yao C, Gu M. [Clinical study of Bio-Oss powder and Bio-Oss collagen for site preservation during implantology]. Shanghai Kou Qiang Yi Xue. 2020;29(4):414-7. Chinese.
Stavropoulos A, Bertl K, Spineli LM, Sculean A, Cortellini P, Tonetti M. Medium- and long-term clinical benefits of periodontal regenerative/
reconstructive procedures in intrabony defects: Systematic review and network meta-analysis of randomized controlled clinical studies. J Clin Periodontol. 2021;48(3):410-30. doi: 10.1111/jcpe.13409
Cortellini P, Tonetti MS. Improved wound stability with a modified minimally invasive surgical technique in the regenerative
treatment of isolated interdental intrabony defects. J Clin Periodontol. 2009;36(2):157-63. doi:10.1111/j.1600-051X.2008.01352.x
Durwin A, Chamberlain H, Garrett S, Renvert S, Egelberg J. Healing after treatment of periodontal intraosseous defects. IV. Effect of a
non-resective versus a partially resective approach. J Clin Periodontol. 1985;12(7):525-39. doi: 10.1111/j.1600-051x.1985.tb01387.x
Nevins ML, Camelo M, Lynch SE, Schenk RK, Nevins M. Evaluation of periodontal regeneration following grafting intrabony defects with bio-oss collagen: a human histologic report. Int J Periodontics Restorative Dent. 2003;23(1):9-17.
Liu B, Ouyang X, Kang J, Zhou S, Suo C, Xu L, et al. Efficacy of periodontal minimally invasive surgery with and without regenerative
materials for treatment of intrabony defect: a randomized clinical trial. Clin Oral Investig. 2022;26(2):1613-23. doi: 10.1007/s00784-021-04134-w
Levine RA, Saleh MH, Dias DR, Ganeles J, Araújo MG, Renouard F, et al. Periodontal regeneration risk assessment in the treatment
of intrabony defects. Clin Adv Periodontics. Forthcoming 2023; doi:10.1002/cap.10254.
Cortellini P, Cortellini S, Tonetti MS. Papilla preservation flaps for periodontal regeneration of molars severely compromised by
combined furcation and intrabony defects: retrospective analysis of a registry-based cohort. J Periodontol. 2020;91(2):165-73. doi: 10.1002/JPER.19-0010
Trevisiol L, Nocini PF, Albanese M, Sbarbati A, D'Agostino A. Grafting of large mandibular advancement with a collagen-coated bovine
bone (Bio-Oss Collagen) in orthognathic surgery. J Craniofac Surg. 2012;23(5):1343-8. doi: 10.1097/SCS.0b013e3182646c3a
Jung EH, Jeong SN, Lee JH. Augmentation stability and early wound healing outcomes of guided bone regeneration in peri-
implant dehiscence defects with L- and I-shaped soft block bone substitutes: a clinical and radiographic study. Clin Oral Implants Res.
;32(11):1308-17. doi: 10.1111/clr.13830
Sanz-Sánchez I, Sanz-Martín I, Ortiz-Vigón A, Molina A, Sanz M. Complications in bone-grafting procedures: classification and
management. Periodontol 2000. 2022;88(1):86-102. doi:10.1111/prd.12413
Downloads
Published
Versions
- 2024-02-07 (3)
- 2024-02-07 (2)
- 2024-02-07 (1)
Issue
Section
License
Copyright (c) 2024 Journal of Applied Oral Science

This work is licensed under a Creative Commons Attribution 4.0 International License.
Todo o conteúdo do periódico, exceto onde está identificado, está licenciado sob uma Licença Creative Commons do tipo atribuição CC-BY.

